 NASH is a diagnosis showing up more and more in primary practices these days. The main reason is the epidemic of OBESITY. NASH is on the upper end of a spectrum of disorders called Non Alcoholic Fatty Liver Disease (NAFLD). Other end of the spectrum is the relatively benign Hepatic steatosis.
NASH is a diagnosis showing up more and more in primary practices these days. The main reason is the epidemic of OBESITY. NASH is on the upper end of a spectrum of disorders called Non Alcoholic Fatty Liver Disease (NAFLD). Other end of the spectrum is the relatively benign Hepatic steatosis.
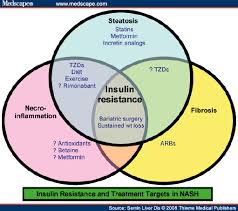
NASH comprises heaptic steatosis associated with necrosis and inflammation. The main pathophysiology behind NASH is 1. Insulin resistance leading to.... 2.Hyperinsulinemia and 3. increased free fatty acids. Also implicated are oxidative injury due to induction of CYP450 in these pts. An evidence to show insulin resistance as a cause is a study comparing incidence of NASH in Type1 Vs type2 diabetics....showing a significantly higher incidence in the latter.Due to above pathophysiology..it is common to find NASH in patients with metabolic syndrome.
Usually patients with NAFLD do not have specific symptoms from the disease. They might complain of malaise, lethargy, nausea etc. Its rare to have right upper quadrant pain or jaundice. What they will have is a slightly elevated AST /ALT (< 4 x normal..and ALT > AST). So we are not going to jump to this diagnosis straight away in this scenario. The first and important thing to exclude is the presence of alcoholic liver disease. (History..history..history!!). then we round the usual suspects(viral hepatitis, toxins, drugs etc). But its reasonable to suspect NAFLD in pts..with above characteristics without alcohol exposure...in the first place
.The risk factors are the same as for met syndrome- Obesity(prevalant in 75% of pts with body wt >10% of ideal!), Diabetes type 2, hypertriglyceridemia, equally present in males Vs females ( but likelihood of fibrosis is increased in females). Because of this association....pts with NAFLD have an increased cardiovasscular risk...have a look at this EASL statement 2008 & a latest abstract from a study on adolescents with obesity(Am J of Epi 2010)Imaging can show fatty liver.Liver biopsy is the only tool that can differentiate a benign steatosis to NASH. 8-20% of obese individuals with hepatic steatosis will have NASH..........and risk of development of fibrosis and cirrhosis from NASH is 10-50%. NASH leading to cirrhosis is the cause for 1% of liver transplantations.
Management is going to be the same as for metabolic syndrome----loosing weight, improving insulin sensitivity( Metformin & Pioglitazone are modestly effective in reducing the fat in the liver..and improving the histology in diabetic pts...and less so in non diabetic pts).Urodeoxycholic acid which was previously used as treatment...is no longer recommended..due to lack of efficacy as shown in this randomised trial ( Hepatology 2004)The latest trial published in NEJM May 2010, was on Vitamin E . Vit E @ 800 IU /day showed a significant improvement in NASH histology(mainly in no diabetics), improvement in liver enzymes..without any benefit on development of fibrosis. It will be reasonable to have these pts on Vit E (but remember that Vit E @ high doses have shown to increase mortality!).....All these measures are aimed at improving inflammation in the liver....but whether these will result in a mortality benefit..remains to be known.
This was grreat to read
ReplyDelete